
How has caregiving in America changed? For starters, more caregivers are adopting technology to help them address the complex and challenging workflow. Unfortunately, more caregivers are reporting that their own health has declined. As caregiving due to COVID-19 restrictions increases, tech-enabled solutions must be prioritized.
By Jane Sarasohn-Kahn, MA, MHSA
The profile of caregivers in America is changing: They’re younger, more financially strapped and taking on more medically oriented tasks, according to the Caregiving in the U.S. 2020 study from The National Alliance for Caregiving (NAC) and the AARP.
On the promising front, caregivers have started to adopt technology that addresses the increasingly complex and challenging workflow of caregiving. In these times of COVID-19-impacted social distancing, tech-enabled caregiving can deliver a human touch—without the potential negative side effects.
The AARP has conducted the Caregiving in the U.S. study since 1997. The 2020 update is the AARP’s fifth detailed profile on caregiving in America.
The key headline here is that caregivers’ own health has eroded in the five years since the 2015 report was written.
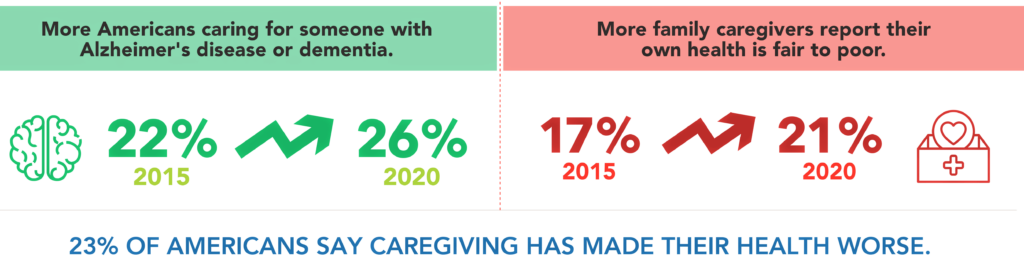
In 2015, 17% of caregivers said their own health was fair to poor. This rose to 21% in 2020. Nearly one-fourth of caregivers found it hard to take care of their own physical health.
Two key factors that changed from 2015 to 2020 contribute to caregivers’ health eroding:
- More caregivers are caring for two or more recipients, increasing from 18% in 2015 to 24% in 2020.
- More caregivers are caring for adults with more complex challenges, such as additional comorbidities as the cared-for population ages, as well as growing mental health and memory problems. The longer a caregiver provides care, the more likely they take on support tasks of advocating, monitoring health and communicating with clinicians.
One of the roles of caregiving is helping manage the costs of care. One in four caregivers reported that it was difficult to get affordable services in their local area. Thus, financial health is also a stress on caregivers—28% of caregivers have stopped saving, 23% have taken on more debt and 22% have consumed their liquid savings. One in five caregivers have unpaid bills or pay them late.
The AARP developed the Level of Care Index in 1997’s Caregiving in the U.S. study to measure the intensity of caregivers’ individual circumstances. The index is constructed from the caregivers’ hours of care and number of activities of daily living (ADLs) and instrumental activities of daily living (IADLs) performed.
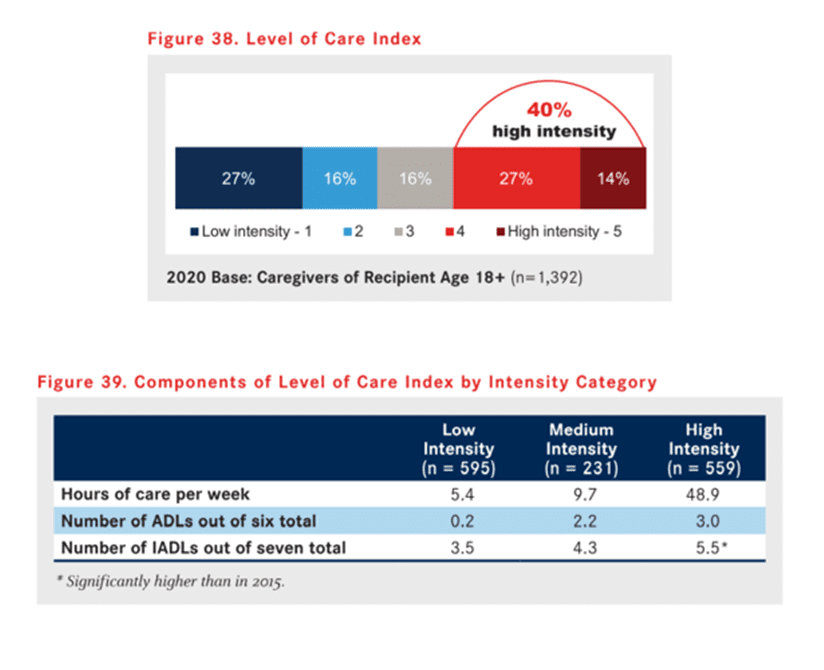
Note that 40% of caregivers report high-intensity levels of care. The chart shows that at the highest level of caregiving, the caregiver devotes nearly 50 hours per week and provides at least eight activities to support their loved ones.
Clearly, caregivers’ workflows have become more complex and diverse. They cover the traditional role of supporting activities of daily living; the increasing demands for organizing the instrumental activities of daily living like transportation, grocery shopping and administering medications; and a growing burden of managing finances for both personal and medical purposes.
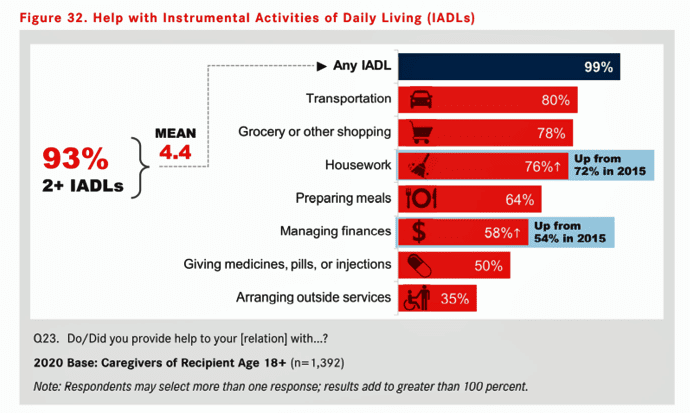
Caregiving for IADLs is the project management of everyday life, shown in the bar chart above—buying groceries, arranging rides, and managing money and outside services. Furthermore, half of caregivers are providing the “medical activity of daily living,” such as administering medicines or injections to those for whom they care.
Given the complexity caregivers face, they seek advice and skill-building across a range of the daily living demands they support: how to keep their loved ones safe at home, how to manage emotional stress, how to manage paperwork, identifying activities to do with their loved ones, and other important ongoing tasks.
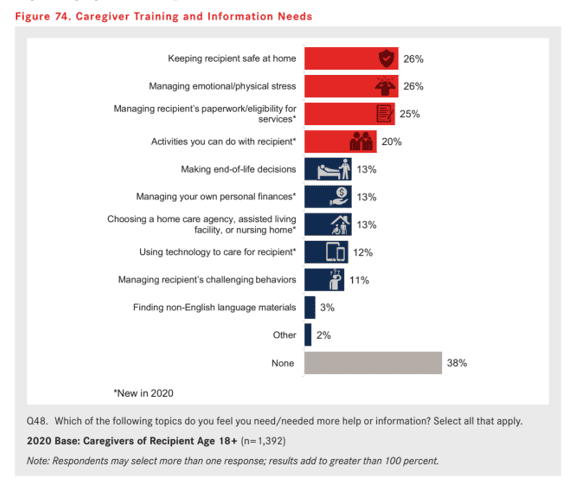
Four in five caregivers currently get this kind of advice, most likely from physicians and healthcare professionals, friends and family. Caregivers rely less on hospitals, government agencies or organizations focused on care for the aging.
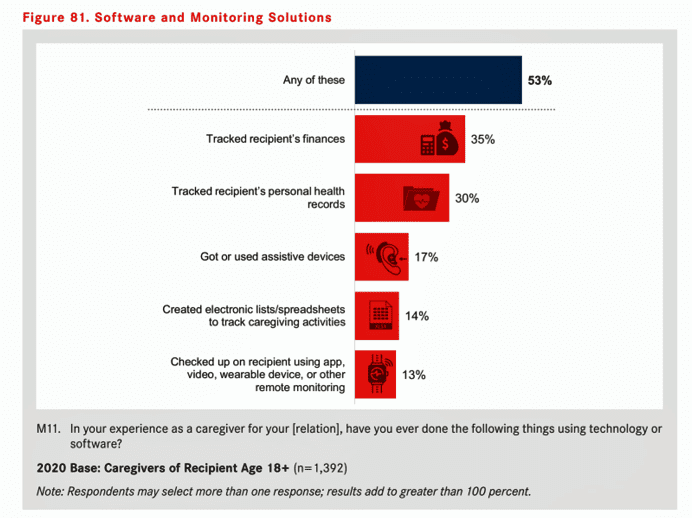
A growing go-to source for caregivers’ support comes from technology. One-half of caregivers have used some form of software or monitoring solution, most commonly to track the finances of the cared-for (35%) or to track personal health records (30%). In addition, 17% accessed or used an assistive device; 14% created an electronic list to track caregiving activities; and 13% checked up on their loved one using an app, video, wearable device or other remote tracking tech.
The study found that caregivers who had a higher level of intensity of effort were more likely to use these technologies, as were caregivers who felt alone, those with greater financial stress, and those with a memory or mental health issue to deal with.
Three in five caregivers went online to support their caregiving effort. The most common workflows were to seek online sources for support services, to manage prescription refills, to place an online order for groceries or household supplies, or to watch videos to learn how to perform different tasks for the cared-for. About 1 in 10 caregivers connected with caregiving peers using social media.
In the current era of the coronavirus pandemic, caregiving has taken on a new dimension: “we’re relying on friends and family to care for the older adults and people living with disabilities in our lives,” C. Grace Whiting, JD, president and CEO of the National Alliance for Caregiving, said in a press release about the study.
COVID-19 is reshaping our collective lives across ages and stages of American life: our physical health, our financial, and our mental and emotional states, which I discussed last month.
In their respective industry segments, including healthcare stakeholders from health plans and health systems to pharma, life science companies and retail health, all serve the caregiver. Increasingly, caregivers will look for advice, support services, and products that help streamline care and support evermore challenging, complex and costly workflows for caring. The AARP/NAC research suggests many opportunities to serve caregivers and the people they love, through creating technology supports backed with enchanting design and empathy.
“Ultimately, caregivers are us,” the report concludes. “Together, we can develop and enact solutions to support family caregivers and to improve their well-being and the well-being of those for whom they provide care.”
Nothing speaks more for Medecision’s mantra of Liberating Healthcare than meeting caregivers at this moment.



About The Author: Jane Sarasohn-Kahn, MA, MHSA
Through the lens of a health economist, Jane defines health broadly, working with organizations at the intersection of consumers, technology, health and healthcare. For over two decades, Jane has advised every industry that touches health including providers, payers, technology, pharmaceutical and life science, consumer goods, food, foundations and public sector.
More posts by Jane Sarasohn-Kahn, MA, MHSA