
Long after we flatten the curve, Americans will still be dealing with lingering mental health issues.
By Jane Sarasohn-Kahn, MA, MHSA
While one-half of Americans are anxious about contracting the coronavirus, even more—two-thirds—are worried about their loved ones becoming seriously ill or dying from COVID-19, the American Psychiatric Association (APA) discovered in a study of peoples’ perspectives on their mental health in the pandemic.
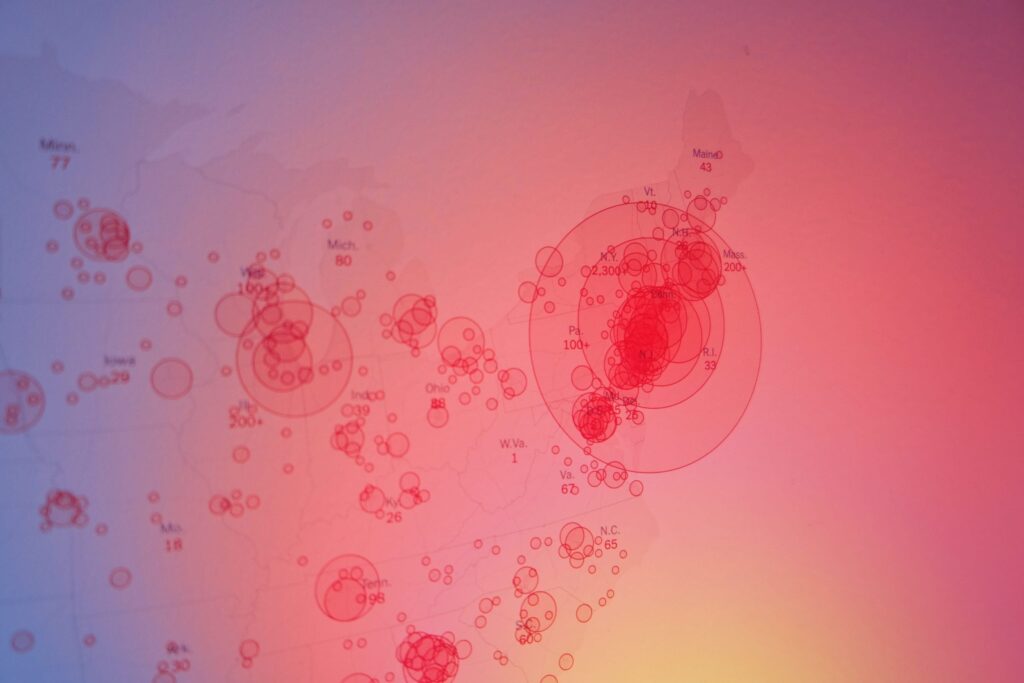
In the U.S., the COVID-19 pandemic is exacting several shocks to the American public: the clinical impact of the virus itself; the #StayHome mandate requiring physical distancing and both staying at and working from home, 24/7; and negative financial impacts due to job loss, hours cut from work, and a large working cohort in the gig economy finding itself without work.
Long after local COVID-19 curves flatten and medical bills from the pandemic are outsourced to collection agencies, Americans will be dealing with mental health impacts that will persist. Anxiety, depression, loneliness and increased incidents of domestic violence are among a host of impacts that may not be seen—but they will surely be felt by more people than perhaps at any other time in U.S. public health history.
That’s because the pandemic has impacted virtually everyone—young and old, male and female, regardless of socioeconomic status and ethnicity. Stress and anxiety will be the great mass-levelers of U.S. well-being in 2020.
Most Americans viewed coronavirus as serious, and a majority worried about contracting the virus on March 5, 2020. That day, APCO Worldwide conducted a poll of 1,000 U.S. adults at the front end of the pandemic, summarized in a research brief aptly titled United States of Anxiety.
From a consumer standpoint, people driven by fear began to take “extreme measures,” Wunderman Thompson Intelligence observed, with panic-buying and stockpiling cleaning products, health protection supplies and nonperishable food becoming mainstream behavior. The new-normal behaviors in America were exercising less, cooking at home more and streaming entertainment services inside our homes.
 Most people in areas mandated to “shelter in place” complied with that instruction, en masse. Eighty-two percent of people became concerned about leaving their home. By April, most people in the U.S. were avoiding public places, heeding the urging of state level officials and the three trusted scientific advisers on the White House Coronavirus Task Force: Dr. Anthony Fauci, Dr. Deborah Birx and Surgeon General Dr. Jerome Adams, who united in a frequently broadcast public service announcement to #StayHome. That phrase became a trending Twitter hashtag in the coronavirus social media moment.
Most people in areas mandated to “shelter in place” complied with that instruction, en masse. Eighty-two percent of people became concerned about leaving their home. By April, most people in the U.S. were avoiding public places, heeding the urging of state level officials and the three trusted scientific advisers on the White House Coronavirus Task Force: Dr. Anthony Fauci, Dr. Deborah Birx and Surgeon General Dr. Jerome Adams, who united in a frequently broadcast public service announcement to #StayHome. That phrase became a trending Twitter hashtag in the coronavirus social media moment.
By Holy Week 2020, many Jews celebrating Passover and Christians celebrating Easter Sunday found solace in using videoconferencing technology to convene. Jews held Zoom Seders; virtual Easter Sunday invitations on Evite increased 1,130% since last year.
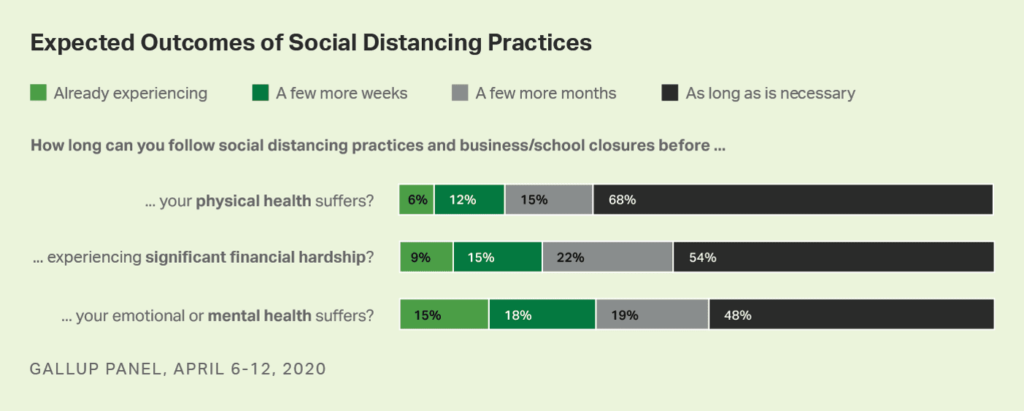
Physical distancing has taken a toll on Americans across three lenses on personal health: physical, financial and mental, the Gallup poll found. By the second week of April, more Americans felt their emotional or mental health was suffering ahead of their physical or fiscal wellness.
 The coronavirus pandemic will exacerbate these trends.
The coronavirus pandemic will exacerbate these trends.
Nearly one-half of U.S. adults felt that their worry or stress due to the coronavirus was having a negative impact on their mental health, growing week by week as the pandemic’s diagnoses increased across the U.S., Kaiser Family Foundation’s research revealed in its early April health tracking poll. More women than men were feeling the negative impact on mental health, as well as more people of color.
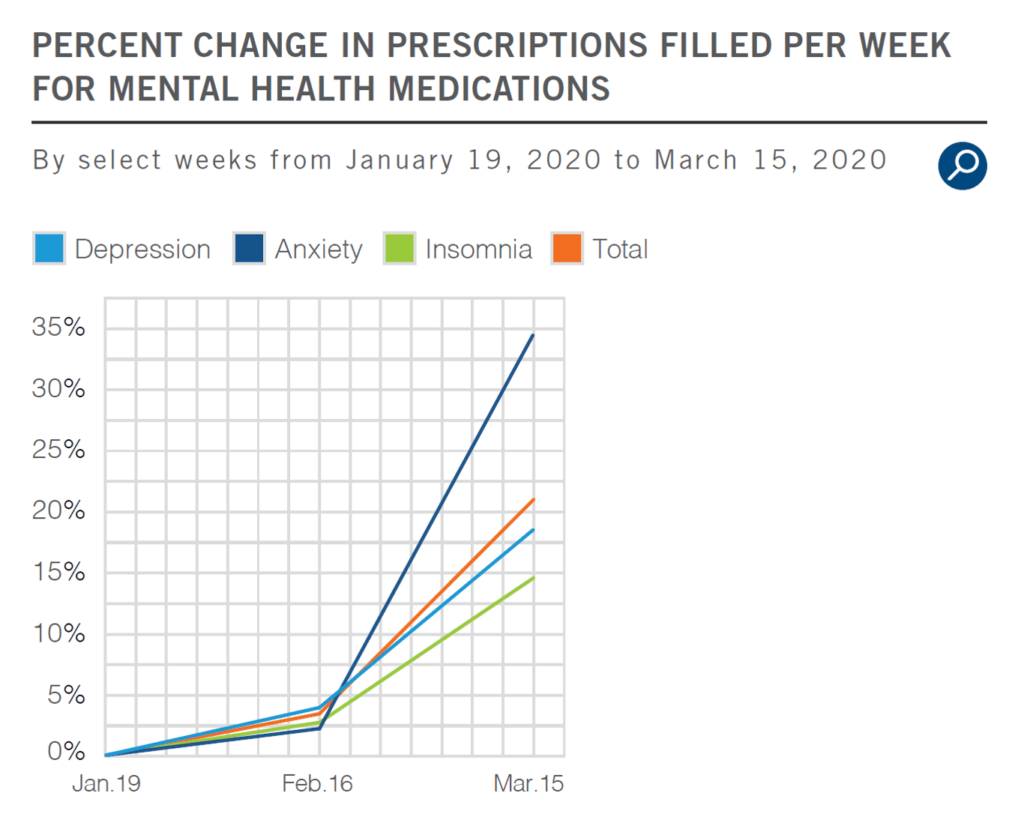
![]() Between mid-February and mid-March 2020, Express Scripts found that the COVID-19 pandemic had already impacted mental health in America as expressed through the volume of antidepressants and anti-anxiety and anti-insomnia medicines prescribed—with Rxs increasing by 21% over the four weeks. Among the three categories of mental health meds, prescriptions written for anti-anxiety drugs grew most dramatically at 34%—from a 12% decline in use from 2015 to 2019. The PBM’s report, America’s State of Mind, tracked how the pandemic was negatively shaping the mental health of patients in the first phase of the crisis.
Between mid-February and mid-March 2020, Express Scripts found that the COVID-19 pandemic had already impacted mental health in America as expressed through the volume of antidepressants and anti-anxiety and anti-insomnia medicines prescribed—with Rxs increasing by 21% over the four weeks. Among the three categories of mental health meds, prescriptions written for anti-anxiety drugs grew most dramatically at 34%—from a 12% decline in use from 2015 to 2019. The PBM’s report, America’s State of Mind, tracked how the pandemic was negatively shaping the mental health of patients in the first phase of the crisis.
 With the recognition that COVID-19 will have mental health impacts beyond physical ones, affecting more people than those directly infected by the virus, healthcare providers, plans and collegial industry stakeholders have an expanded role to play to address this issue that will be the epidemic after the pandemic.
With the recognition that COVID-19 will have mental health impacts beyond physical ones, affecting more people than those directly infected by the virus, healthcare providers, plans and collegial industry stakeholders have an expanded role to play to address this issue that will be the epidemic after the pandemic.
Even though Express Scripts’ core business is drug therapies, its report calls out “what’s next in treatment” as a technology opportunity—telehealth’s moment to scale tele-mental health.
“Telehealth programs for the treatment of mental health have been on the rise and offer several advantages,” Express Scripts asserts. “They provide access to healthcare practitioners for mental health assessments, counseling, patient education and monitoring that might otherwise not be feasible.” This is especially important in rural areas, Express Scripts says, and other geographies with clinician shortages.
The APA urged the Centers for Medicare and Medicaid Services (CMS) to expand its regulation of tele-psychiatry to include patients with older phones that lack a video camera or broadband access to receive therapy and medication management from physicians. “Even if we can’t physically see our patients … we must be able to provide care to our patients in a way that respects current guidelines on social distancing,” APA wrote to CMS. APA’s research has found that some of the frailest patients and many with serious mental illness face obstacles of care because they lack smartphones or live in areas without broadband access, or they cannot afford it.
I wrote a paper for California HealthCare Foundation in 2008 titled Right Here, Right Now: Ten Telehealth Pioneers Make It Work. In the paper, I told the story of Dr. Jay Sanders, who worked with the Medical College of Georgia in 1993 on what the team termed “the electronic house call.” To enable that reimagined house call, they leveraged a piece of consumer electronics mainstream in patients’ homes: a television. “The reason we wanted to use the TV was we wanted it to be totally intuitive for the person,” Dr. Sanders said.
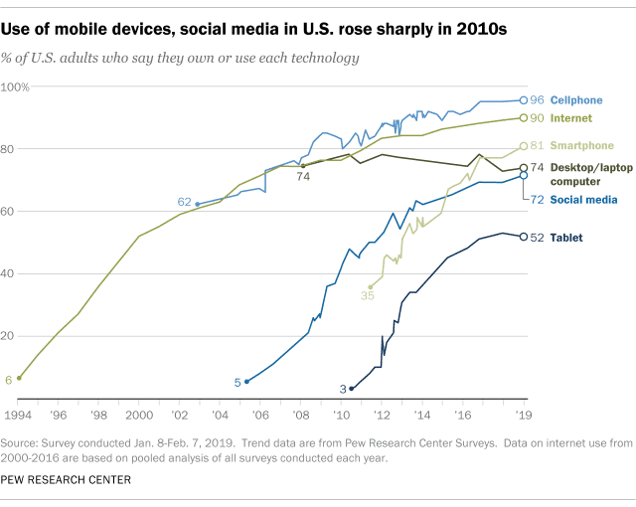 Today, that universal consumer electronics platform is the mobile phone, owned by at least 4 in 5 U.S. adults in 2019, according to the Pew Research Group. One-half of Americans also had a mobile tablet in 2019, with fully 9 in 10 people able to access the Internet.
Today, that universal consumer electronics platform is the mobile phone, owned by at least 4 in 5 U.S. adults in 2019, according to the Pew Research Group. One-half of Americans also had a mobile tablet in 2019, with fully 9 in 10 people able to access the Internet.
The ubiquity of these mobile platforms people use in everyday life has enabled people in the #StayHome pandemic era to stream entertainment, Zoom holiday rituals with family members far afield, and use ecommerce to build up pandemic pantries and hygiene supplies.
These platforms also enabled patients at home to stay out of the doctor’s office and emergency department to convene with a health professional in the earliest phase of the COVID-19 crisis. In late March 2020,1 in 3 people in the U.S. had used a digital channel to communicate with a health professional in the previous weeks.
Patients’ demand for virtual visits represents Americans’ “appetite for healthcare evolution,” APCO Worldwide noted in another consumer study conducted in late March 2020. Nine in ten Americans thought it likely that more healthcare services would be available remotely or virtually in 2021 as a direct result of the pandemic, and 6 in 10 people said they’d be likely to use these services.
Among the most exposed people in the COVID-19 pandemic are healthcare professionals, who were highlighted in a JAMA opinion piece published April 7. In the essay, the three doctor-authors offer this table that details “requests” from clinicians to their organizations during the current crisis. These are to: “hear me, protect me, prepare me, support me and care for me.”
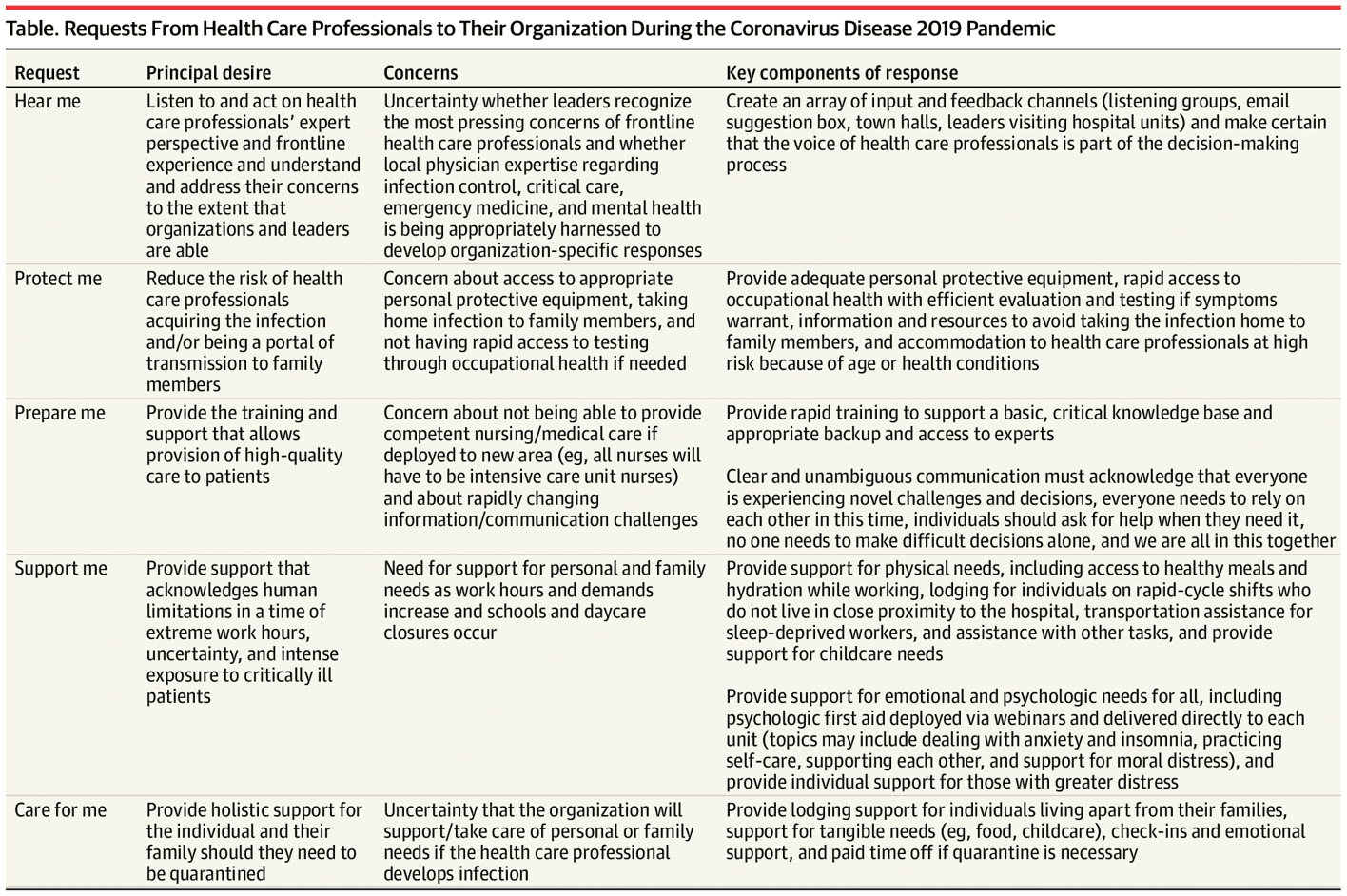
Providers are patients, too—and these five requests can inform how health industry stakeholders can approach how to partner with all patients to recognize and bolster mental health for all.
Looking toward 2021, two-thirds of Americans expect to confront shortages of mental health providers to address the consequences of social distancing, APCO found. And surely, in 2021, U.S. healthcare professionals like those described in the JAMA essay will feel more burned out, anxious and depressed—signs already present in the Medscape 2020 physician survey on emotional health.
With that forecast, patients and clinicians are telling us, humbly and honestly, that they’ve diagnosed their collective growing need for mental health support in the coronavirus era and its aftermath. It is incumbent on health system industry players to collaborate and meet the moment to address mental health as, simply, health. This is an overwhelmingly clear opportunity, and challenge, gifted by the coronavirus pandemic.

About The Author: Jane Sarasohn-Kahn, MA, MHSA
Through the lens of a health economist, Jane defines health broadly, working with organizations at the intersection of consumers, technology, health and healthcare. For over two decades, Jane has advised every industry that touches health including providers, payers, technology, pharmaceutical and life science, consumer goods, food, foundations and public sector.
More posts by Jane Sarasohn-Kahn, MA, MHSA