How can health plans help providers cross prior authorization hurdles? We give four strategies.
By Medecision
Used effectively, prior authorization is a tool designed to protect healthcare providers, patients and payers by reducing costs and verifying the need for, and appropriateness and safety of, a medication or procedure for a given patient. Unfortunately, it too often becomes a burden that creates unnecessary red tape, unnecessary redundancy, confusion and misunderstanding.
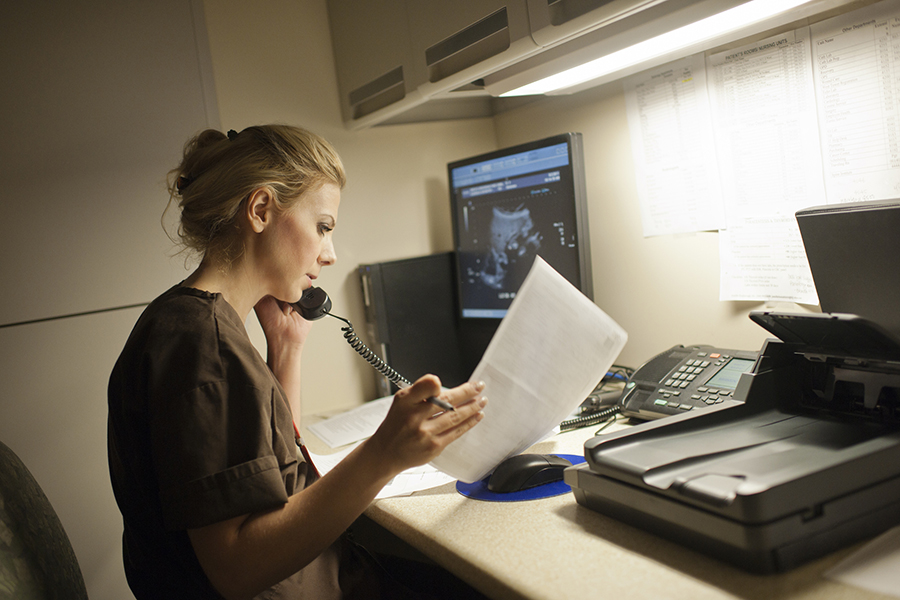
That is because prior authorization remains a largely manual process—one that is often still completed via fax or phone. It’s also complex. For example, for a hip replacement surgery, a payer might require ICD-10 codes, three months of office visit notes, documentation of the patient’s symptoms, imaging results, documentation of conservative treatment within the last year, exam findings and documentation of any active infection.
A Complex Process
This complex process costs physicians a lot of time. A 2021 survey from the American Medical Association (AMA) revealed that physicians and their staff spend an average of almost two business days each week completing prior authorizations. The survey also found that, on average, practices complete 41 prior authorizations per physician, per week.
Prior authorization is necessary—its ultimate goal is to improve patient outcomes by ensuring a patient receives the most appropriate treatment. But the manual process that involves checking for prior authorization requirements, contacting the health plan, reviewing the patient information, and ultimately denying or approving the order can take days or even weeks when completed by fax and manual entry.
In January 2021, the Centers for Medicare and Medicaid Services (CMS) passed the “Interoperability and Prior Authorization” final rule, which promotes data sharing, more patient access to personal information, coordinated care and interoperability to make the prior authorization process more efficient. The proposed rule is scheduled to go into effect on January 1, 2023. The proposed rule applies to a select group of CMS payers including Medicare Advantage organizations, Medicaid managed care plans, state Medicaid agencies, children’s health insurance program (CHIP) agencies, CHIP managed care entities, and issuers of qualified health plans on the federally facilitated exchanges.
“The prior authorization rule is really about making sure that people get the right treatment for the right cost—and without delay,” said Julie Barnes, founder and principal at Maverick Health Policy, in a 2021 webinar hosted by Medecision.
Ways to Simplify Prior Authorization
In the meantime, however, simplifying the prior authorization process for providers and patients is critical. Read on for four strategies payers can use to increase the efficiency and effectiveness of the prior authorization process.
- Reevaluate services that need prior authorizations. In a poll conducted on May 18, 2021, by the Medical Group Management Association, 81% of medical groups said that payer prior authorization requirements have increased since 2020. Consider limiting prior authorizations to include only services that require medical necessity or policy reviews—and eliminating requirements for routine care and procedures.
- Leverage electronic tools to make the process easier. Medical practices contract with multiple health plans—and each payer has its own set of requirements and rules for prior authorization. Often, providers and their staff will create “cheat sheets” to keep track of all the rules—but this means they may not be up-to-date on any policy changes. Electronic tools can help providers and their office staff know when prior authorization is required for a procedure and what documentation is necessary.
- Accelerate with automation. The slow-moving prior authorization process can have an impact on patients’ health, the AMA survey results suggest. Of the physicians surveyed, 34% reported that prior authorization has led to a serious adverse event for a patient in their care. When asked how often the process delay impacts patients’ access to necessary care, 42% of physicians said often, 38% said sometimes and 14% said always. Payers should consider solutions that can automate the process where possible, streamlining tasks, reducing administrative costs and speeding response times.
- Be proactive. As previously mentioned, medical practices complete 41 prior authorizations per physician, per week. For a practice with 10 physicians, that’s 410 prior authorizations per week—and 1,640 per month. Only 40% of physicians have staff who work exclusively on prior authorizations. Payers can alleviate the burden on physicians and their staff by being proactive and sending status updates and follow-up communications so that providers know the status of an authorization.
To learn more about the benefits of automating authorizations to improve efficiency, download our Piedmont Community Health Plan success story. In it, you’ll learn how Piedmont used Aerial™, Medecision’s HITRUST CSF®-certified, SaaS solution, to automate authorizations and improve efficiency—reducing prior authorization turnaround times by 57%.



About The Author: Medecision
Fully delivering on the promise of data — and making the business of healthcare simpler and more successful — Medecision offers a whole new world of possibilities. The company's flagship offering, Aerial™, stands as the market's most extensible clinical data platform. It offers complete contextual awareness of members and automates next best actions — simple campaigns, complex care management, utilization approvals, and more — for optimal health outcomes.
Aerial is not only quick to deploy, it is easy to manage. The platform's effectiveness in reducing both medical and administrative costs, coupled with its role in improving the member and patient experience, has made it the preferred choice for health plans and care delivery organizations. Presently, Aerial is instrumental in catering to over 10% of the U.S. population, marking a significant milestone in advancing healthcare efficiency and effectiveness.
More posts by Medecision